What is gastroparesis?
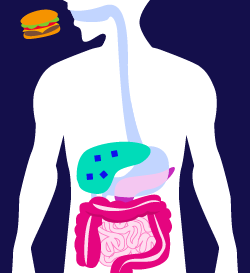
Gastroparesis is a condition where the movement of the muscles in the stomach is slowed down or halted completely. Ordinarily, your stomach relies on muscle contractions to move food through your system—this is also called motility. With gastroparesis, inadequate motility may prevent your stomach from effectively emptying.1
What causes gastroparesis?
The exact cause of gastroparesis is often unclear, but people living with type 1 diabetes and type 2 diabetes may develop it as a complication of their condition. Varying blood glucose levels can damage your vagus nerve, which controls your stomach muscles. Since your stomach depends on the vagus nerve to move food through your digestive tract, blockages and even bacterial infections can occur if it’s not working properly.2
Symptoms of gastroparesis
The most common symptoms of gastroparesis can make everyday life a challenge. Individuals with gastroparesis may experience the following symptoms:
- Nausea
- Vomiting
- Bloating
- Discomfort in the abdominal area
- Heartburn
- Loss of appetite
- Weight loss
- Feeling prematurely full
- Significant variability in blood glucose
If you are experiencing these symptoms, you should consult with your doctor immediately. In some cases, however, gastroparesis shows no symptoms at all, especially in the initial phase of the condition.
Complications of gastroparesis
For people with diabetes, gastroparesis can cause serious complications. If your stomach is not moving food as it should be, the rate at which you absorb glucose becomes unpredictable, which can make managing your blood sugar difficult.
Other complications can include:
- Dehydration
- Malnutrition
- Bezoars (undigested masses of food that harden in the stomach)
Treatment options

About 20 percent of people with type 1 diabetes will experience gastroparesis. It’s also more common in women than men. There is currently no cure for gastroparesis, but it is most commonly treated with medication or by regulating your blood sugar levels.
Dietary changes can also go a long way in controlling gastroparesis3. A doctor or dietitian may recommend consuming more starches, proteins, or certain fruits and vegetables- blended/strained if necessary, as they have been shown to effectively manage this condition.
Other helpful dietary changes can include:
- Eating smaller meals at more frequent intervals
- Avoiding alcohol and carbonated drinks
- Adequately chewing your food
- Drinking 1 to 1.5 liters of water per day
- Lightly exercising after you eat
Research continues to find new ways to treat and medicate gastroparesis. If you are currently living with this complication due to diabetes, consult with your doctor to see what treatment options are right for you.
2. Gastroparesis. The Global Diabetes Community Page. https://www.diabetes.co.uk/diabetes-complications/diabetes-and-gastroparesis.html. 18AUG2021
3. Gastroparesis: Diagnosis & Treatment. The Mayo Clinic Page. https://www.mayoclinic.org/diseases-conditions/gastroparesis/diagnosis-treatment/drc-20355792. Accessed 18AUG2021
Looking for more tips? Join the list
Subscribe to our newsletter, News to Infuse, and receive monthly diabetes tips and helpful information.