A Day in the Life: Type 1 Diabetes vs. Without Edition
Living with type 1 diabetes versus without
Thanks to advanced technology like automated insulin delivery (AID) systems, managing diabetes today is easier than it’s ever been. But make no mistake — living with type 1 diabetes is still a full-time job.
What people without diabetes may not realize is the daily vigilance, multiple calculations, and all the invisible decisions that shape the life of someone living with diabetes. Check out what a typical day in the life is like for Bruce, who lives with type 1 diabetes and manages it with AID, compared to Jane, who’s not living with diabetes.
Morning: Waking up
After the first alarm goes off (typically followed by a few hits of that snooze button)! This is how Bruce and Jane’s morning might go:
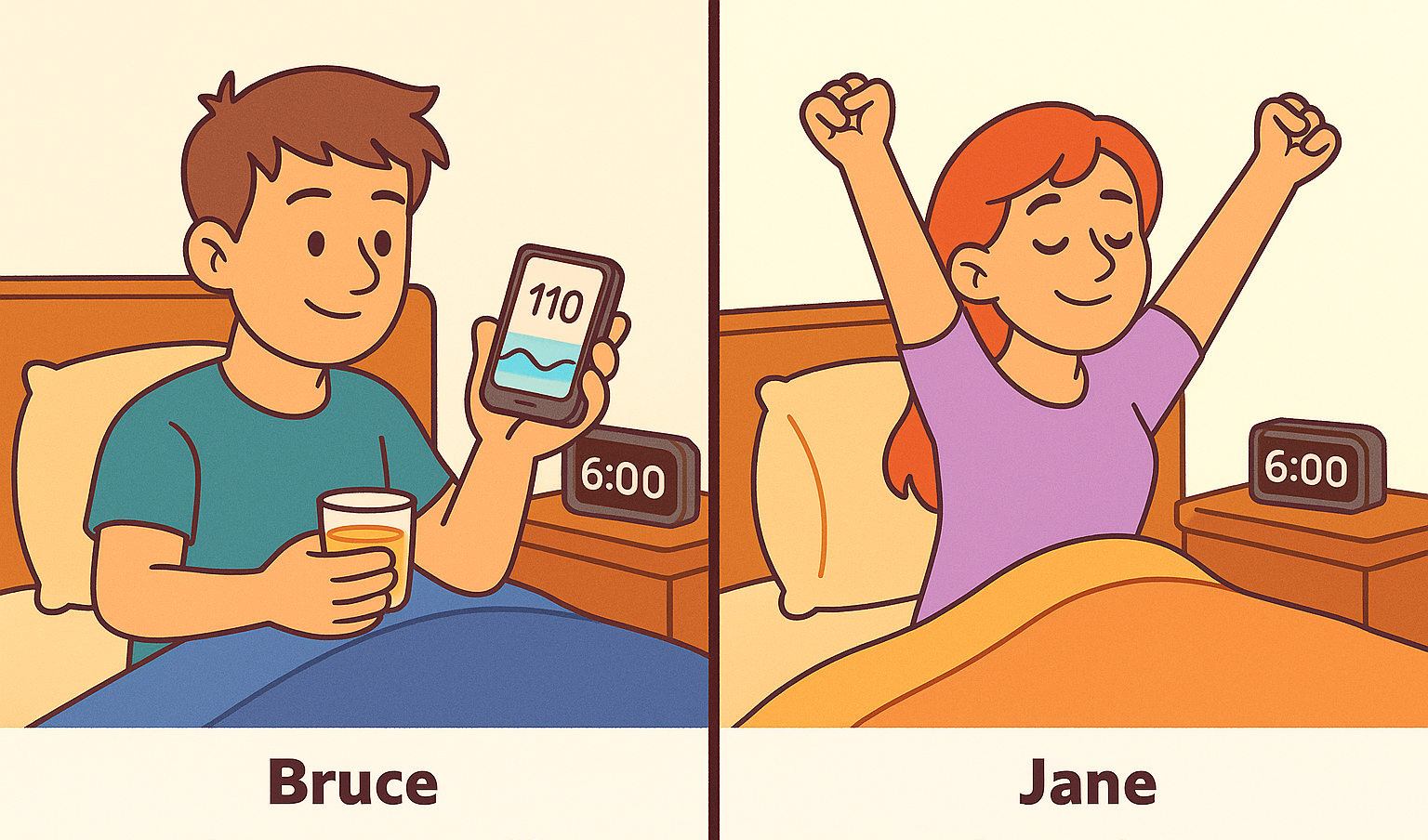
Bruce (T1D)
Alarm goes off.
Checks CGM reading on phone or pump. Sees a stable overnight trend (thanks to auto corrections!),† still reviews it.
Drinks a sip of juice and makes a slight correction.
Jane
Alarm goes off.
Stretches.
Scrolls on phone.
Showers.
Breakfast
They say breakfast is the most important meal of the day, but it’s even more so when you’re trying to keep your blood sugar in range.
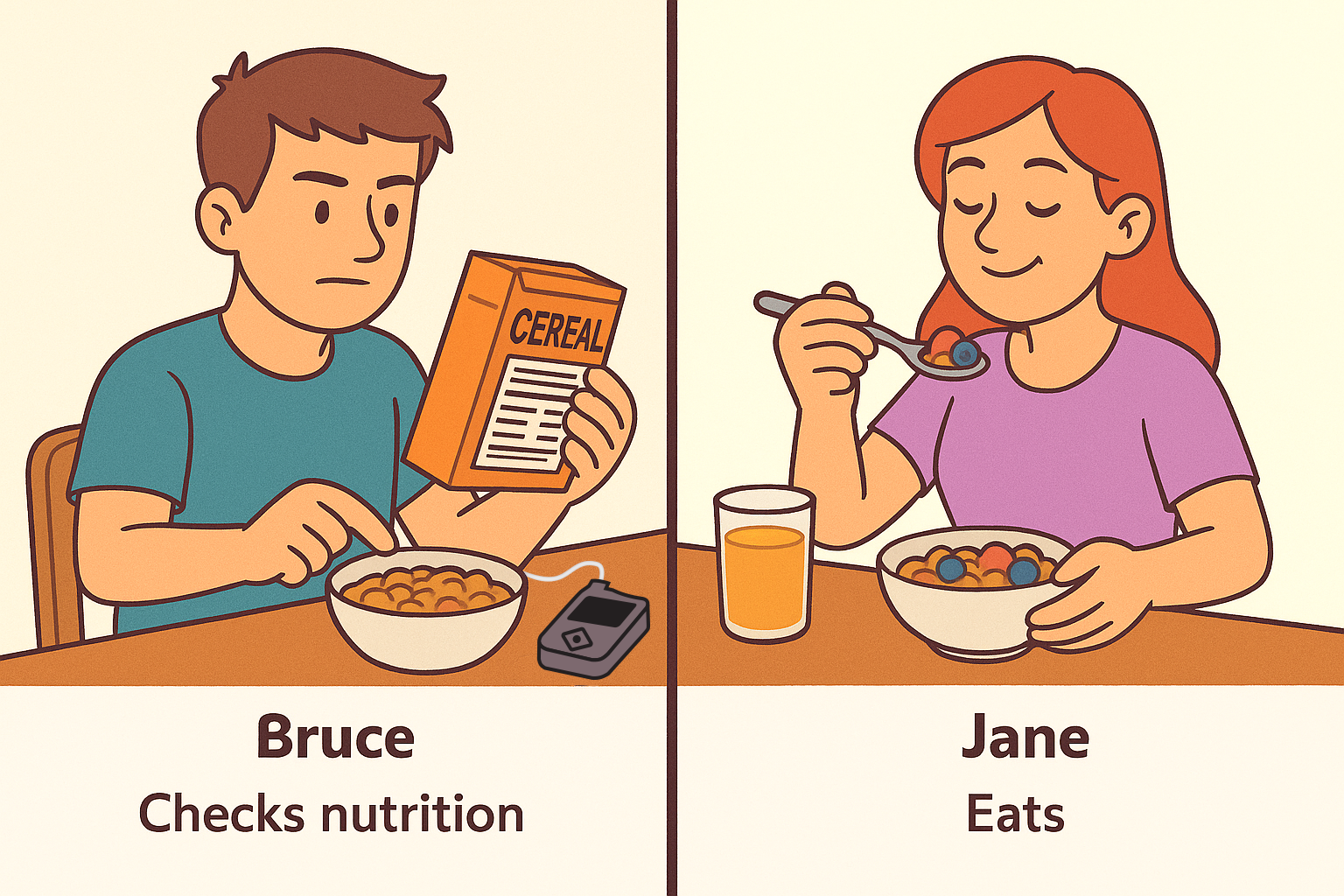
Bruce (T1D)
Checks carb content.
Doses insulin.
Waits a bit before eating.
Keeps an eye on CGM graph.
Jane
Pours cereal, adds fruit.
Eats while checking email or chatting with a partner.
Commuting to work
If you got the RTO (return to office) memo, you’re now on the highway heading to work. Mostly uneventful, unless you experience a high in the middle of traffic.
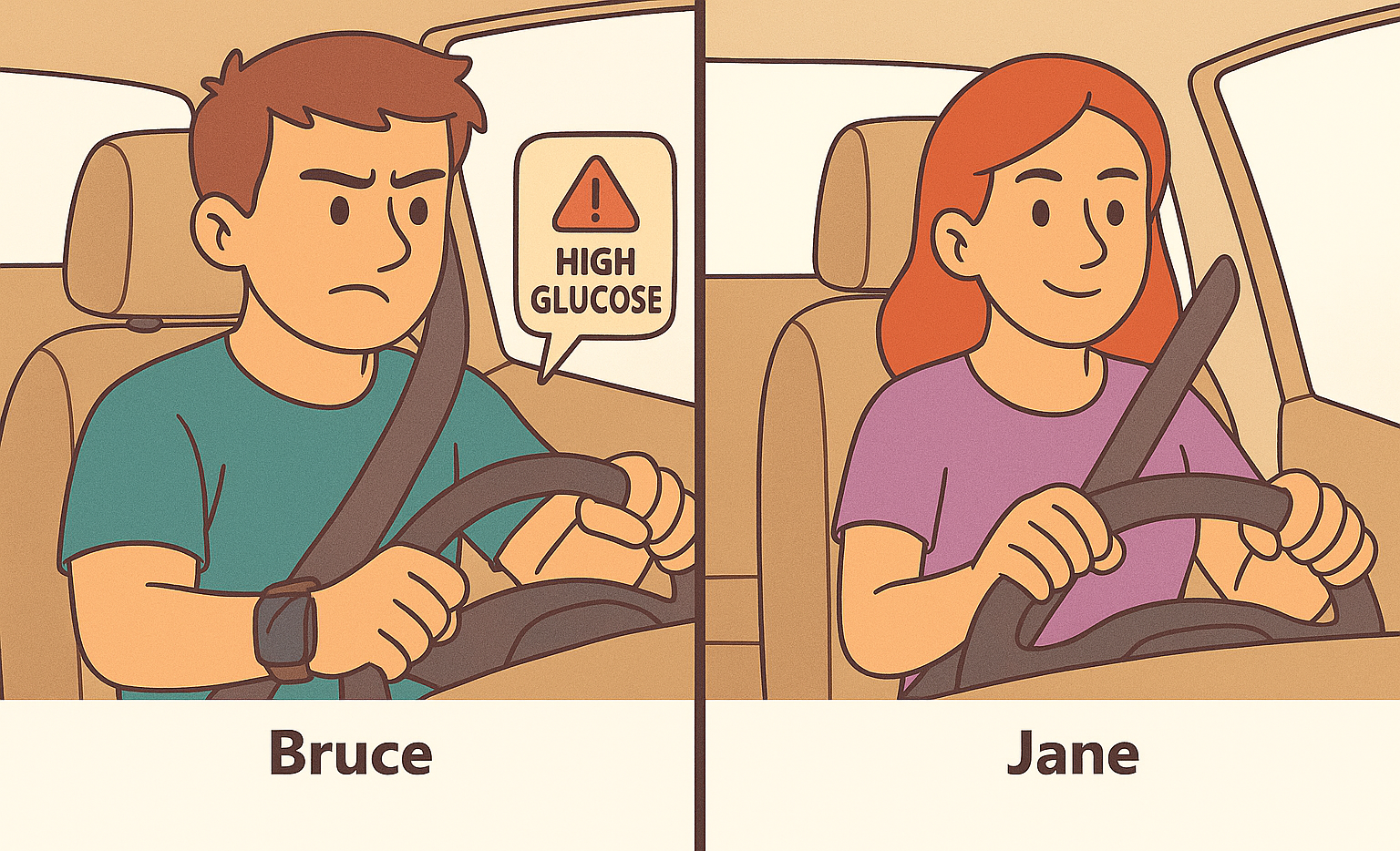
Bruce (T1D)
Walk, drive, or bus.
Podcast time.
Sees alert on smartwatch.
Pump is already correcting breakfast high. Sips water.
Jane
Walk, drive, or bus.
Podcast time.
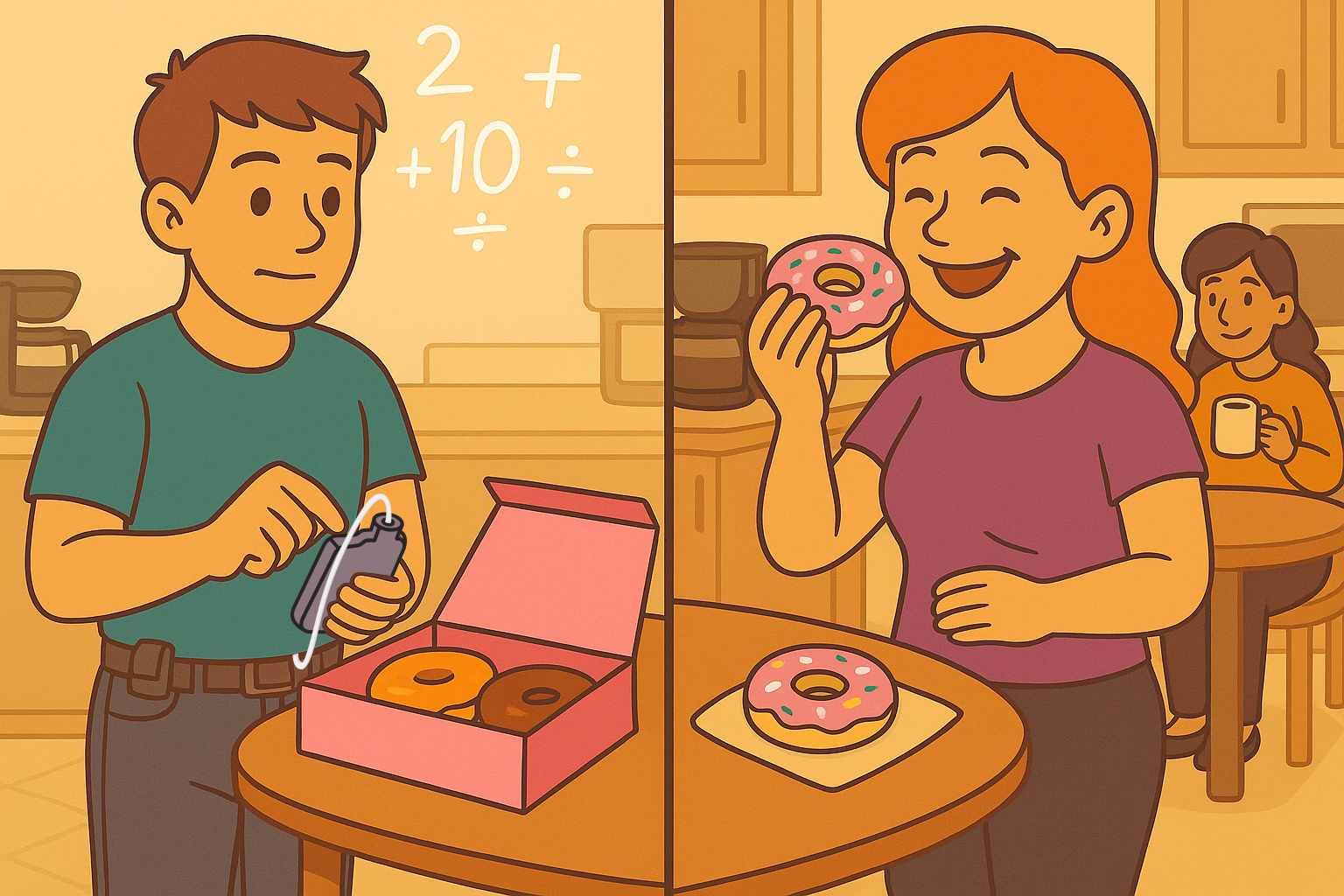
At the office: Donuts!
Your team did an amazing job last quarter, and the boss treated everyone to some sweet, delicious donuts in the breakroom! Decisions, decisions...will it be a classic glazed or the one with pink frosting and rainbow sprinkles? If you’re like Bruce and need to count carbs to bolus, there might be another calculated decision in store.
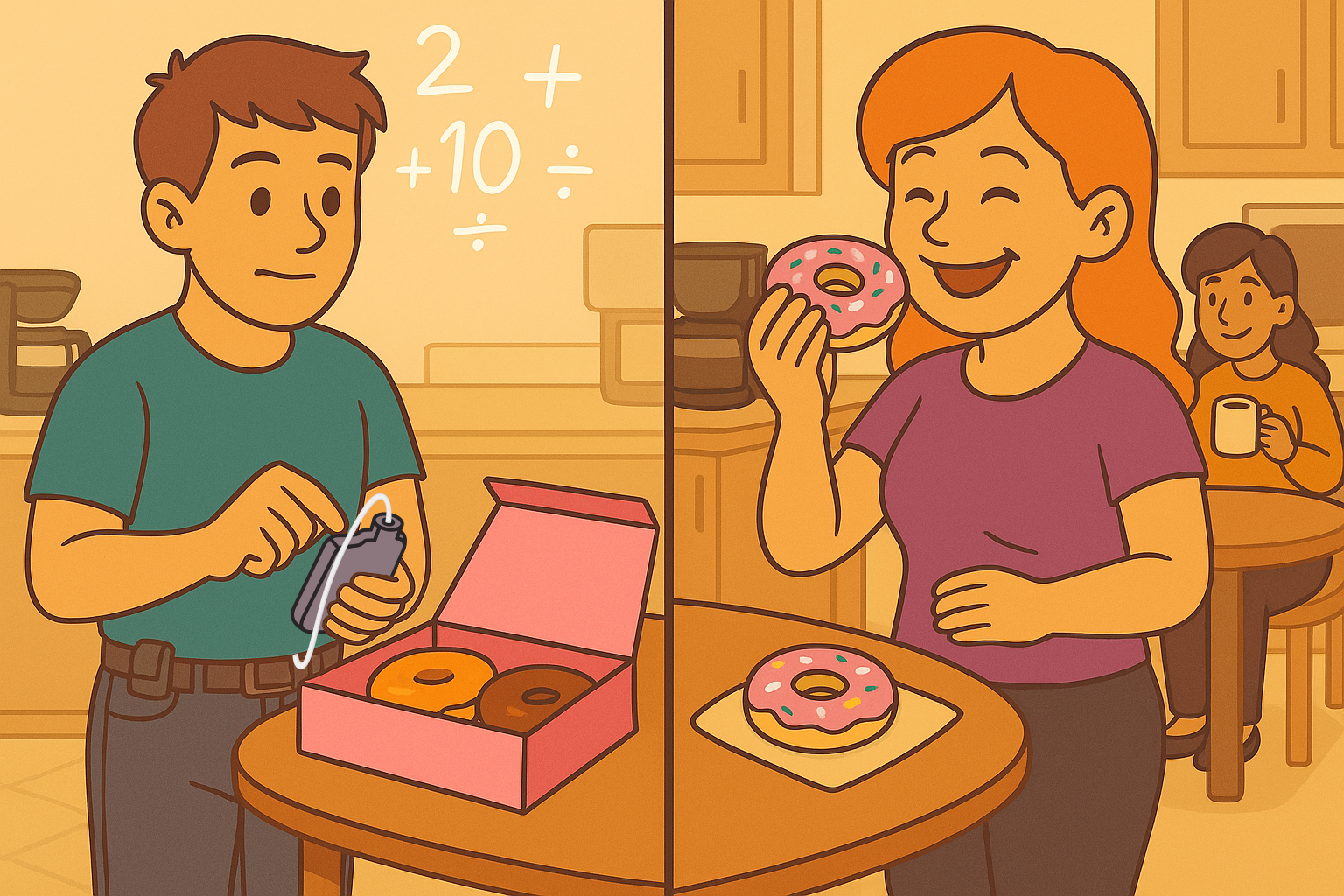
Bruce (T1D)
Pauses. Checks glucose levels.
Boluses via pump.
Pump will adjust if needed later.
Grabs a donut.
Jane
Grabs the one with pink frosting and sprinkles — no extra thought required.
Lunch with coworkers
Everyone is going to lunch together and they invite you to eat at a local burger joint. Your first thought is either “How many carbs are in hamburger buns again?” or “I wonder if they have sweet potato fries?”
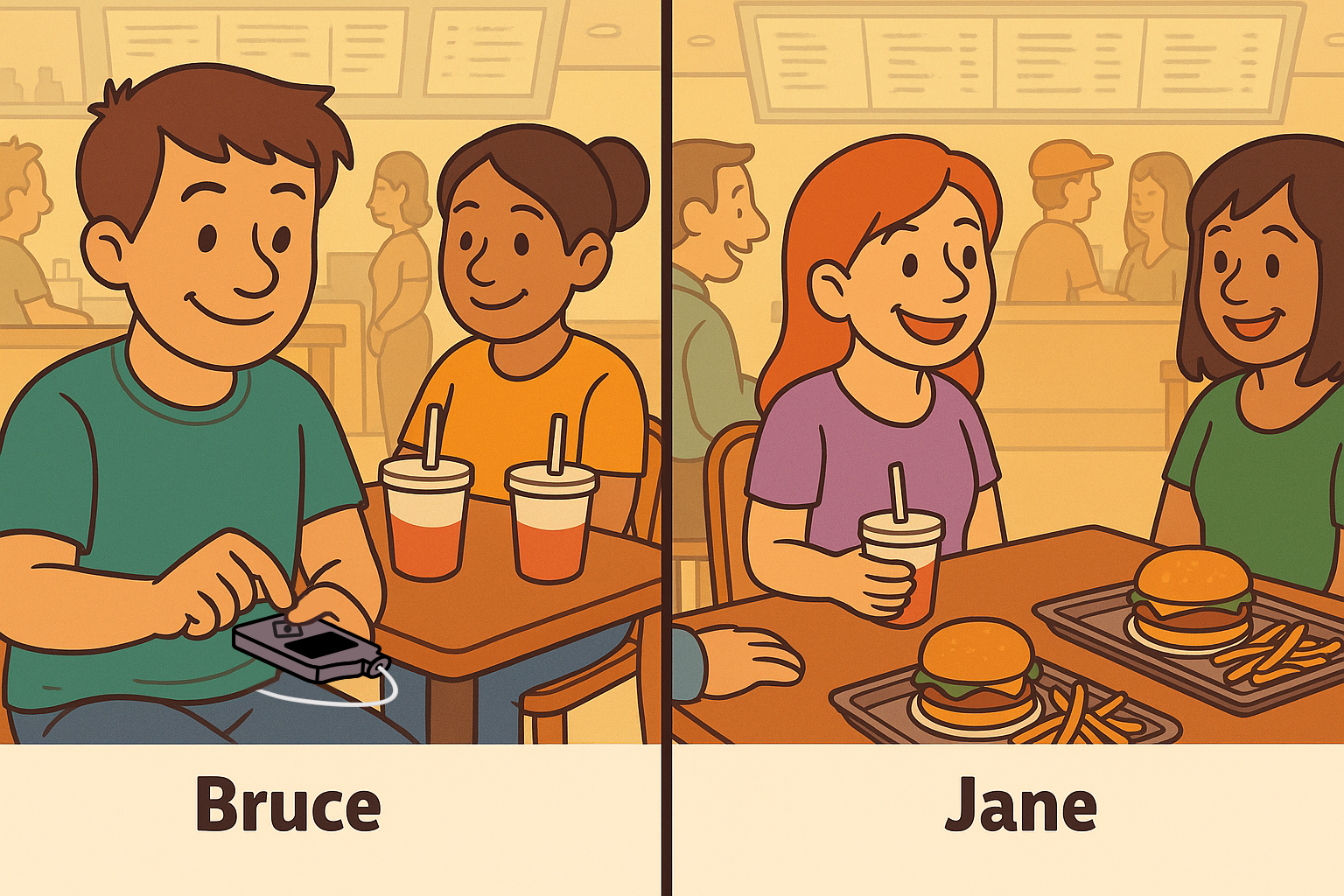
Bruce (T1D)
Orders a cheeseburger and sparkling water.
Enters carbs into his pump.
Tries to pre-bolus, but food comes out late. Watches sugar levels while chatting.
Jane
Orders a cheeseburger with a side of sweet potato fries and a Coke.
Eats right away.
Workout time
Work is over and Bruce and Jane both head to the gym.
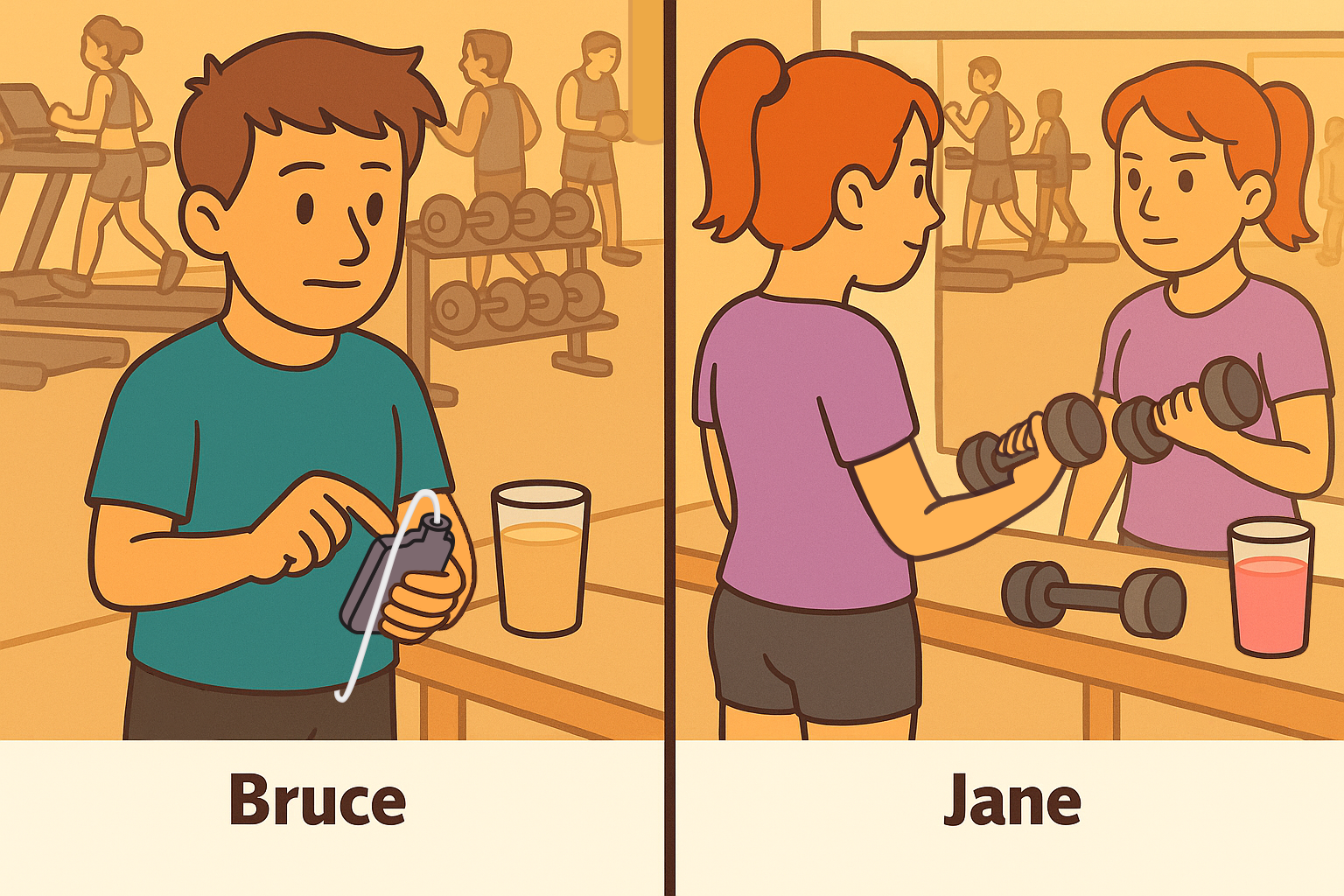
Bruce (T1D)
Turns on temp target an hour before his workout.
Brings fast carbs along just in case.
Checks CGM.
Starts workout.
Jane
Throws on shoes.
Hits the gym.
Dinner
Time to fuel those gains! While one may choose a salad and protein shake in the hope of canceling out that cheeseburger from lunch, the other may choose it to avoid an onslaught of heavy carbs again.
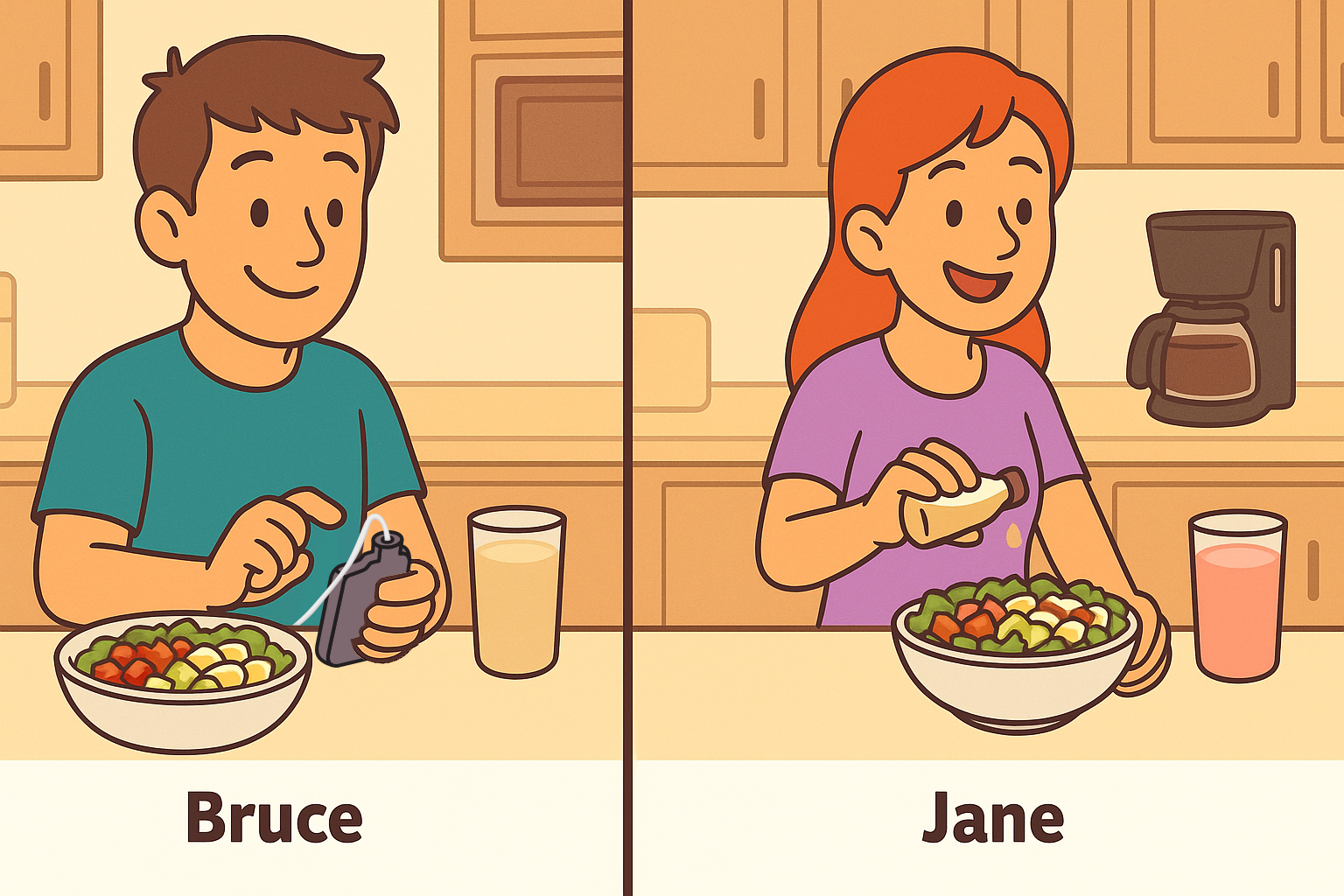
Bruce (T1D)
Enters carbs into pump.
Relaxes and enjoys dinner.
Jane
Relaxes and enjoys dinner.
Bedtime
Time for bed — which often means lying there scrolling on your phone for another hour or two. For Bruce, that just means a little extra prep.
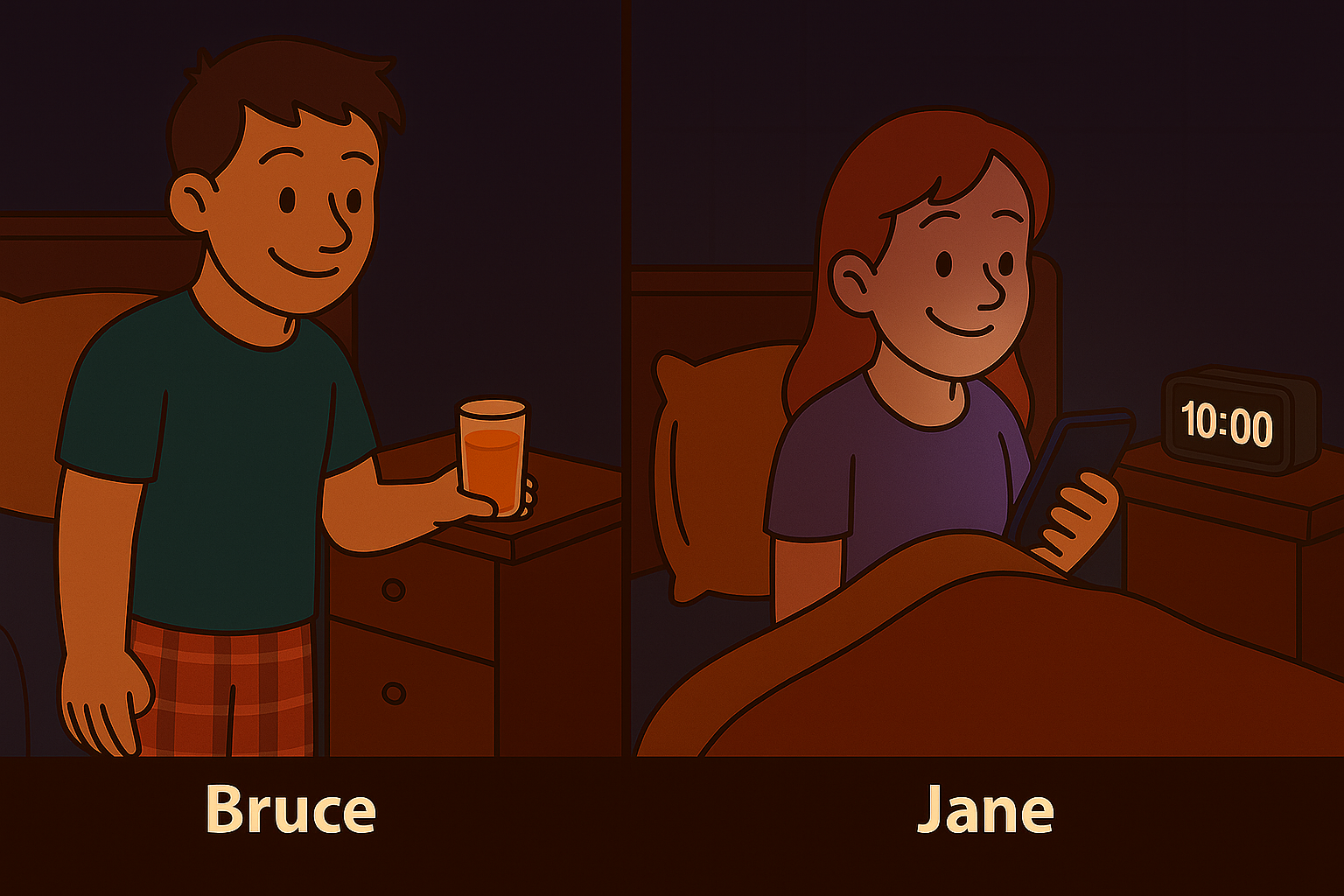
Bruce (T1D)
Brushes teeth.
Puts on PJs.
Places glass of juice on nightstand.
Checks glucose levels.
Sets pump alerts.
Scrolls on phone.
Sleep.
Jane
Brushes teeth.
Puts on PJs.
Scrolls on phone.
Sleep.
If you're living with diabetes, know you're not alone — and you're doing more than most people realize! If you're not, now you have some insight into the whole other world that runs quietly (but constantly!) in the background of the life of a person living with diabetes.
† Refers to SmartGuard™ technology. Individual results may vary.
Note: Images generated using ChatGPT.
Important Safety Information: MiniMed™ 780G system with SmartGuard™ technology with Instinct sensor, Simplera Sync™ sensor, and Guardian™ 4 sensor
The MiniMed™ 780G system is intended for the continuous delivery of basal insulin at selectable rates and the administration of insulin boluses at selectable rates for the management of type 1 diabetes mellitus in persons 7 years of age and older using the Instinct, Simplera Sync™ or Guardian™ 4 sensor, and of type 2 diabetes mellitus in persons 18 years of age and older requiring insulin using the Simplera Sync™ or Guardian™ 4 sensor.
The MiniMed™ 780G System includes SmartGuard™ technology, which can be programmed to automatically adjust insulin delivery based on the continuous glucose monitoring (CGM) sensor glucose values and can suspend delivery of insulin when the sensor glucose (SG) value falls below or is predicted to fall below predefined threshold values. The system is intended for use with connected sensors, including the Simplera Sync™ and Guardian™ 4 sensors and integrated continuous glucose monitors, including the Instinct sensor, each of which has different wear-time, form factor, insertion site, and other distinguishing characteristics that relate to sensor performance. Consult the appropriate sensor user guide when using the system. Discuss treatment decisions with your HCP.
WARNING: Do not use the SmartGuard™ feature for people who require less than 8 units or more than 250 units of total daily insulin per day. A total daily dose of at least 8 units, but no more than 250 units, is required to operate in the SmartGuard™ feature. |


