Dealing with diabetes distress

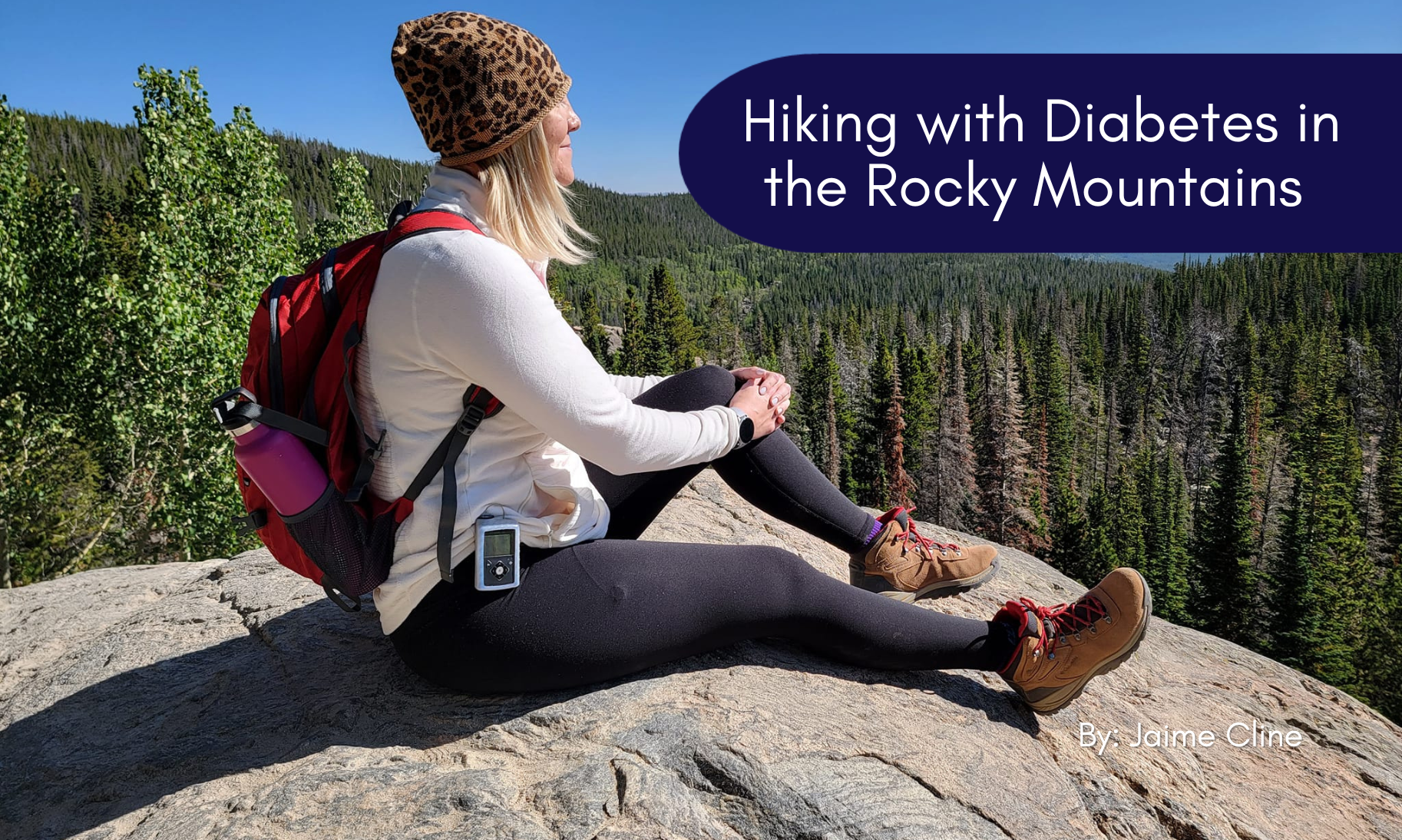
Pursuing your vision of ideal health as a person with diabetes is not always a straight path. There are ups and downs all along the way. Sometimes a down period makes sense—you may be having a hard time keeping up with treatment or external factors could be affecting your health. But, on other occasions, down times feel entirely unpredictable. You can be doing all the right things, only to see your blood sugar spike or plummet randomly.
When you’ve dealt with these unpredictable shifts, you know it can be upsetting. If you’ve experienced periodic downturns when diabetes feels more difficult to manage, you might begin to experience “diabetes distress” – and yes, this is a real thing!
What is diabetes distress?
Diabetes distress can feel a lot like burnout. It can cause frustration, sadness, anxiety, and guilt— especially if people continuously hammer home the importance of self-care. While everyone who wishes to help might have good intentions, it can be hard for others to understand the mental weight of managing diabetes.
As you might have already experienced, diabetes distress can make it harder to keep up with your treatment schedule, compounding self-management difficulties and exacerbating other diabetes stress symptoms. But stopping that chain reaction before it begins can help. Here are some of the signs you might be experiencing symptoms of diabetes distress:
- Frequently feeling anger and frustration about the physical and mental demands of treatment
- Feeling overwhelmed and worried about treatment progress but feeling powerless to stop it
- Purposely or subconsciously avoiding doctor appointments and blood sugar checks to avoid bad news
- Feeling isolated and lonely
- Frequently making unhealthy dietary and fitness choices out of desperation
- Continually worrying about future complications
No matter what, we hope that you understand these feelings are not atypical and don’t represent personal failing. Distress is exceptionally common—about 36 percent of people with type 2 diabetes have reported significant distress, along with an estimated 20 to 40 percent of people with type 1 diabetes. Diabetes distress is even more common for those who take insulin.
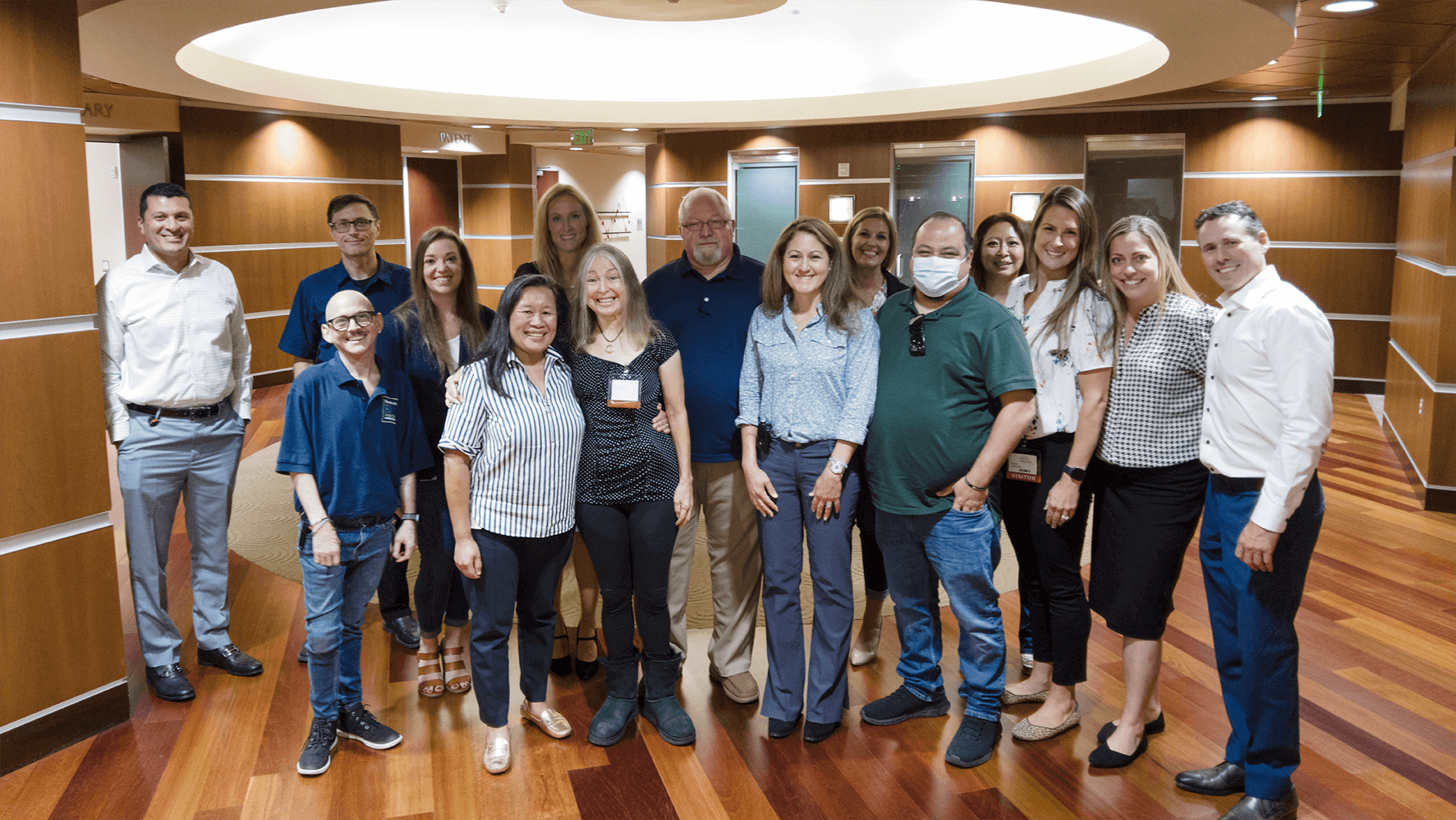
How your doctor can help
Your closest contact with knowledge of the intricacies of your treatment is your doctor or your healthcare team. And studies have shown that the way you interact with your doctor is critical to preventing diabetes distress in the first place. One-on-one interactions with your doctor should include good communication that helps to develop a positive relationship. This can improve self-care outcomes and give you more confidence that you can follow their suggestions and recommendations. Having the right healthcare team around you is key!
If you’re experiencing diabetes distress, it’s important to have support from a diabetes care professional who will work closely with you to figure out a game plan to get back on track. Having positive reinforcement, encouragement, and creativity in finding the right solutions can help set you up for success.
Steps to prevent diabetes distress
You can take steps to keep yourself from burning out throughout the course of your treatment. Here are a few tips that can help when you feel hopeless or overwhelmed:
- Always take time to pay attention to how you’re feeling. Burnout can be subtle, so you may not notice it unless you allow yourself space to gather your thoughts. If you are feeling any of the previously mentioned symptoms for more than a week, talk to your doctor about diabetes distress to see what they can do to help.
- If your distress is related to a lack of resources, pharmacists and healthcare providers can likely recommend programs that can help you pay for the costs of your crucial medicines, especially insulin.
- While family and loved ones may not know what it’s like to be in your shoes, talk to them about how you’re feeling. Even just being honest about your frustrations can help to lessen their effects on your treatment and state of mind.
- Look into additional avenues if you still need help. The CDC has a list of resources available for individuals experiencing distress or financial difficulties.
There is no reason to take on diabetes distress alone. In fact, knowing there are programs and professionals out there who want to help and who understand the importance of mental health may help lessen the feelings of loneliness and despair. If you’ve personally experienced diabetes distress, what are some tips you can share with the diabetes community?